Among all the pathological processes affecting the spine in its various parts, cervical osteochondrosis is considered one of the most common. This disease causes many complications, mainly because it affects the spinal cord and also negatively affects the functioning of the brain.
According to statistics from 2017, the disease has become significantly younger. If previously osteochondrosis mainly affected people after 40 years, today different stages of cervical osteochondrosis are diagnosed in 90% of people over 25 years old. For this reason, it is important to know as much as possible about the pathology, from its nature to treatment methods.

What is cervical osteochondrosis?
In medical practice, the words cervical osteochondrosis mean a progressive acquired disease that affects a specific part of the spine. This pathological process is characterized by degenerative-dystrophic processes in the tissues of the intervertebral discs, which are shock absorbers for the cervical vertebrae.
Degenerative-dystrophic changes in the intervertebral discs are caused by their wear and deformation. As a result, the distance between the vertebrae is reduced and the following consequences occur:
- Narrowing of the spinal canal in certain areas of the spine.
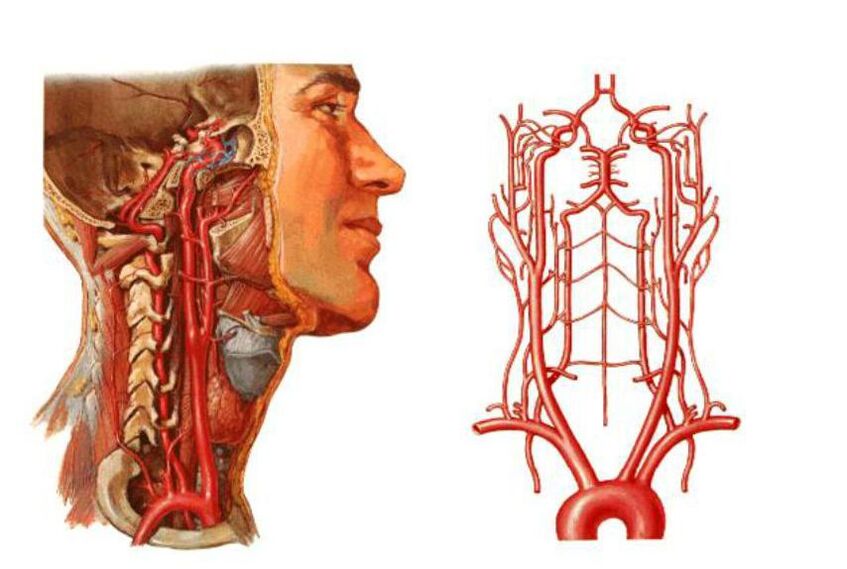
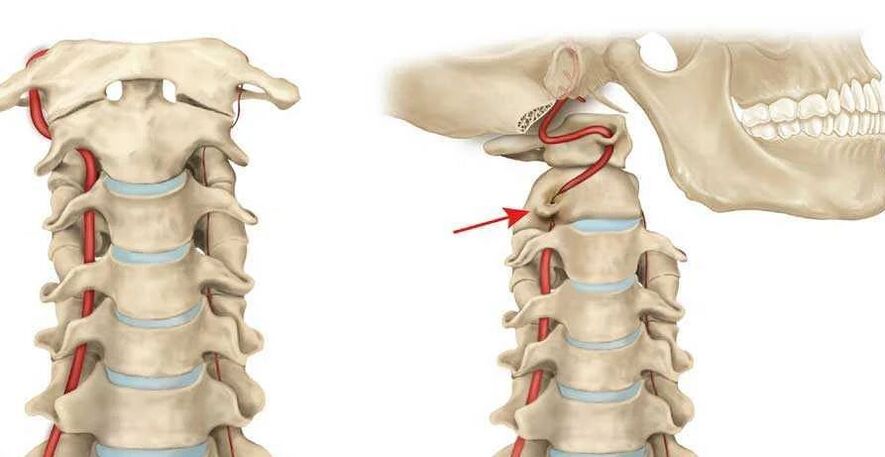
- Compression of the vertebral arteries - large blood vessels that provide blood supply to the brain. As a result, the supply to the brain deteriorates and blood circulation in the cervical spinal cord is disrupted.
- The intervertebral discs can become deformed and flattened. This leads to compression of certain areas of the spinal cord and nerves, most often compression of the nerve roots occurs.
All these problems threaten not only impaired blood circulation in the brain, neck pain, headaches, etc. The development of osteochondrosis of the cervical spine is dangerous due to neurological problems, deterioration of the central nervous system and damage to brain tissue.
According to the international classification of diseases, osteochondrosis of the cervical spine is assigned several separate codes. The disease code according to ICD 10 depends on the age at which the disease was diagnosed:
- M02 – intervertebral disc dystrophy in adolescence.
- M42. 12 – degenerative process in the neck region in adults.
Many factors depend on the age of the patient and the degree of development of the pathological process, for example, the consequences, complications, symptoms and, of course, the principles of treatment.
Causes
Knowledge of the causes of the development of cervical osteochondrosis can play a decisive role in the diagnostic process, as well as in determining the principles of combating the disease.
However, before listing the reasons, it is worth saying that doctors identify two factors that lead to the development of this pathological process:
- Pathological - the destruction of intervertebral discs and other spinal structures with the involvement of neighboring tissues, vessels and nerve bundles in the pathological process occurs under the influence of unfavorable external factors. The more serious these factors and other pathologies are, the faster the disease develops.
- Physiological – the development of pathology is mainly based on age-related changes. We are talking about the natural aging of the cartilaginous tissue of the spine, salt deposits, etc.
If we list the more specific causes of cervical osteochondrosis, they are as follows:
- Disorders of metabolic processes in the body, as well as certain stages of obesity.
- Physical inactivity is a phenomenon characterized by limited mobility. We're not just talking about injuries or illnesses, it also includes a sedentary lifestyle and sedentary work.
- Pathologies of the cardiovascular system that contribute to impaired blood circulation in the brain, pressure changes, etc.
- Poor posture includes various forms of scoliosis, rheumatism and even flat feet.
- Cervical spine injury. In this case we are talking about sprains, blows, bruises. Injuries to other parts of the spine can affect the development of cervical osteochondrosis.
- Excessive physical stress on the cervical spine, caused by intense sports or severe physical difficulties, depending on the person's type of activity.
- A sedentary lifestyle is also dangerous due to constant tension in the cervical spine and throughout the spine if you sit incorrectly or on uncomfortable furniture.
- Hernia of the cervical spine, as well as various concomitant diseases.
- Forced holding of the head for a long period of time in an uncomfortable or unnatural position. In this case, not only muscle tension occurs, but also the spine in the cervical region is curved.
- Doctors consider constant stress and nervous tension to be a very common cause.
- One of the reasons is also considered to be congenital anomalies in the structure of the spine.

What health risks does this pose?
As mentioned previously, the cervical spine region contains not only the spinal cord and various nerve branches, but also the vertebral arteries that supply the occipital portion of the brain, the cerebellum, and the medulla oblongata.
With the development of cervical osteochondrosis, nearby tissues become inflamed. In addition, the development of pathology threatens to compress nerve roots and squeeze blood vessels, the consequences of which are as follows:
- Osteochondrosis is accompanied by deformities of the spine, leading to narrowing of the spinal canal in certain areas. This can lead to compression of the spinal cord and nerve branches, which promises serious neurological problems. In severe cases, a person feels pain and there is even a risk of loss of control over certain parts of the body (mainly the arms or face).
- Compression of the vessels of the neck, as already mentioned, is accompanied by impaired circulation in the occipital region of the brain. In this case, the brain stops receiving oxygen and nutrients in the required quantities and oxygen starvation begins. If blood circulation is impaired, there is a real risk of ischemic stroke and various neurological pathologies.
Syndrome
Speaking about the danger of cervical osteochondrosis as it progresses and lack of proper treatment, the disease can lead to a number of complications and syndromes.
The main syndromes are:
- Vertebral.
- Vertebral artery.
- Koreshkovy.
- Cardiac.
It is important to know that each of these symptoms is accompanied by painful sensations of a different nature, as well as a multitude of unfavorable clinical signs. A person may feel dizzy, have tinnitus and much more.
Vertebral syndrome
Talks about a direct connection between cervical osteochondrosis and bone and cartilage tissues. Symptoms of this type of pathology are also associated with damage to the mentioned tissues:
- Neck movements are partially or completely limited.
- Head movements are accompanied by painful sensations in the neck.
- The x-ray shows morphological changes in the tissues (intervertebral and vertebral bodies).
It should be noted that vertebral syndrome is always accompanied by these three clinical signs. If at least 1 of them is missing, the diagnosis will be completely different.
Vertebral artery syndrome
This syndrome is caused by narrowing of the vertebral artery, which leads to vestibular, vascular and autonomic problems. In this case, the main symptoms are widespread:
- Headaches and migraines.
- Visual impairment.
- Noises in the ears.
- Frequent dizziness and much more.
The most dangerous symptom is fainting, which indicates severe oxygen deprivation.
Radicular syndrome
Occurs when the roots of the spinal cord are damaged. In this case, nerve conduction is disrupted, a person may experience pain or loss of sensitivity in certain parts of the body, or even suffer from paralysis.
Depending on which of the 8 root pairs the conduction disorder occurs, the following symptoms are identified:
- 1 pair – numbness or pain in the back of the head;
- 3rd pair – impaired chewing reflex, numbness of the tongue and unpleasant sensations behind the ears;
- 4 pairs – pain in the clavicle region, impaired swallowing reflex;
- 5 pairs – disorders of the shoulder girdle, accompanied by problems with arm movement;
- 6th pair - the patient begins to feel pain and numbness in the forearm and shoulder blades;
- 7th pair – hands and fingers (usually the index and middle fingers) become numb;
- 8th pair – similar problems to the previous point, but numbness is felt in the ring and little fingers.
Based on the described characteristics, it is sometimes possible to determine which pair of roots is affected by radicular syndrome.
Cardiac syndrome
Despite the fact that the pathological process is still localized in the cervical spine, the syndrome has all the signs of cardiac pathologies. The clinical picture is as follows:
- Rapid impulse.
- Pain in the sternum.
- Shortness of breath, weakness, lethargy, decreased performance.
Degree of development of the disease
When we talk about the degree of osteochondrosis of the cervical spine, we mean the stages of progression of the pathological process, which differ in clinical signs. In total, there are four degrees of development of the disease:
- The first stage is characterized by vague symptoms. Patients complain of mild headaches, and during the first examination, the doctor notices slight muscle stiffness.
- Pain in the cervical spine and head is more frequent, more intense and radiates to the shoulder and arms. The pathology is caused by damage to the intervertebral discs and pinched nerve roots. The pain increases when turning the head, throwing it back and leaning forward.
- In the third stage, the pain is constant, muscle weakness is noted in the arms and hernias form in the intervertebral discs. Movement in the neck area is limited and frequent dizziness is present.
- The fourth stage is accompanied by complete destruction of the intervertebral disc, cartilaginous tissue is replaced by connective tissue. In addition to pain and dizziness, coordination problems are observed and the vertebral arteries are often pinched.
Signs and symptoms of cervical osteochondrosis
To consult a doctor in time, it is necessary to clearly understand the signs of cervical osteochondrosis. In some cases, this knowledge allows you to seek help in the early stages of the disease, when it is easier to treat.
In general, the symptoms of osteochondrosis of the cervical spine are:
- Pain in osteochondrosis is always present, only the intensity and frequency differ. Pain is the first clinical sign. Their intensity depends on the stage of development of the disease, they are dull or compressive in nature. Painful sensations are present mainly in the neck and occipital region, but can also radiate to the temporal region, shoulder girdle and arms.
- In most cases, there are manifestations of damage to the vestibular apparatus. We are talking about frequent and causeless dizziness, nausea, poor coordination of movements, uneven gait, loss of space.
- One of the most common clinical signs is stiffness of the neck muscles and stiffness of movements. It is difficult for a person to turn, lower and throw his head back, the movements are accompanied by attacks of pain.
- Many patients report a feeling of "goosebumps" on the scalp or a characteristic tingling sensation.
- Muscle weakness and numbness occur in the arms.
- Often there are psychological manifestations, expressed by depression, drowsiness, sharp changes in mood, moodiness or irritability.
- Due to poor circulation and damage to brain tissue, dizziness intensifies and noises in the ears appear, similar to rustling, pulsing and buzzing.
- Most patients experience worsening vision, as well as pain in the eyeballs, especially when trying to squint too much to the left, right, up, or down.
It is sometimes possible to determine the degree of development of the pathological process by the symptoms. However, for a complete diagnosis this is still not enough and a number of diagnostic measures are necessary.

Diagnostic methods
Diagnosis of cervical osteochondrosis is necessary to determine the localization and stage of progression of the disease. For a complete diagnosis, the following diagnostic methods are necessary:
- Radiography is the main method for determining the degree and location of spinal deformity.
- Computed tomography can be used to more accurately diagnose pathological changes in the vertebrae and intervertebral discs.
- MRI (magnetic resonance imaging) - allows you to examine the discs and vertebrae in detail, determine the presence of hernias, protrusions, the extent of lesions, etc.
- Dopplerography - with this examination it becomes possible to find the place of compression of the artery and assess the degree of circulatory disorders.
Treatment methods
Treatment of osteochondrosis of the neck always involves an integrated approach. The principles of treatment depend on many factors, such as the age of the patient, the stage of development of the disease, the severity of the clinical picture, etc.
However, you cannot do without a doctor in this situation and you can first contact a general practitioner, who will then refer you to a vertebrologist.
As for the integrated approach: osteochondrosis of the cervical spine is treated using medications, physiotherapy, massage, exercise therapy and other methods, which are worth talking about in more detail.
Medical treatment
The basis of treatment of cervical osteochondrosis is drug therapy, which involves the use of tablets, drugs and drugs from the following groups:

- Analgesics - analgesics and antispasmodics. The former directly blunt the nerve centers, thereby relieving painful sensations. These help relieve neck muscle spasms, improve blood circulation and relieve pain.
- NSAIDs - nonsteroidal anti-inflammatory drugs are necessary to reduce inflammation, most of them also eliminate pain. These medications are often used in the form of gels or ointments that are applied to the affected area.
- Muscle relaxers are another way to relieve muscle spasms in the cervical area.
- Chondroprotectors are obligatory at certain stages of osteochondrosis of the spine, as they contribute to the restoration of bone tissue.
- B vitamins - normalize metabolic processes in nervous tissue, improving the conductivity of nerve impulses and promoting the functioning of the central nervous system.
Remember that treatment should only be carried out under the supervision of a doctor, who is responsible for prescribing each drug, as well as determining the duration of its use and dosage.
Physiotherapy
Treatment of osteochondrosis of the neck will be much more effective thanks to certain physiotherapy techniques:
- Electrophoresis.
- Laser therapy.
- Ultrasound.
- Massage.
Massage therapy must be carried out by an experienced health professional, the treatment is carried out over a period of at least 10 sessions. Cervical massages help normalize blood circulation, restore elasticity, muscle tone, relieve pain, etc.
Physiotherapy
Therapeutic exercises also help speed recovery, but are only performed during recovery stages. It is important that the exercises do not bring discomfort or pain to the patient. Exercise therapy aims to strengthen muscles and relieve discomfort during movement by increasing the elasticity of muscle fibers.
The exercise technique is initially developed by a physiotherapist, and then the patient can practice gymnastics independently at home.
Manual therapy
Manual therapy is based on the principle of restoring motor functions and mobility between the vertebrae. At first, the manipulations consist of a light relaxing massage, then the doctor applies more and more force, applying pressure and rotating the neck towards the vertebrae.
Kuznetsov applicator
The use of Kuznetsov applicators is one of the methods of treating spinal diseases, including osteochondrosis. The effect of the device on the cervical spine normalizes metabolic processes, relieves pain, increases muscle tone, improves blood circulation, increases the conductivity of nervous tissue, etc.
Home treatment
All therapeutic measures are carried out at home, with the exception of physiotherapy, massage (in some cases) and the first stages of exercise therapy. However, now we are talking about traditional medicine and we will consider several of the most effective recipes:
- To use horseradish: take a leaf of this plant, pour boiling water over it and apply the insides to your neck, securing it with a bandage. Can be left in place while you sleep to enhance the effect.
- If there are no contraindications from a doctor, a good remedy would be warming up the cervical spine. The simplest method is to use a pepper dressing, but you can heat the wax cake by applying it 1-2 times until it cools completely.
Disease prevention
To prevent the development of the disease or its return after treatment, it is necessary to prevent osteochondrosis of the cervical spine. It consists of following simple recommendations:
- Sleep on a flat, hard surface, it is better to purchase a special orthopedic mattress and a pillow that fits the shape of your head.
- To prevent disease, monitor your physical activity and do not overload your spine. If you must lift weights, do so gently and keep your back straight.
- If your job requires you to sit for a long time, take breaks. Every hour you need to walk or stretch your stiff muscles with simple gymnastic movements.
To prevent osteochondrosis, it is useful to go swimming and hang on the horizontal bar for 2-3 minutes every day.
























